Psychedelics treatment
Treatments for addiction problems have much in common regardless of the substance. A general, stepwise approach is…
① Stabilisation
② Relapse prevention
③ Lifestyle change
④ Harm reduction
What are the effects of psychedelics?
This is a large group of psychoactive drugs which have similar effects but act on different receptors in the brain. There are three subgroups…
Hallucinogens include LSD, psilocybin, and mescaline which cause sensory disturbances such as brighter colours or sharper sounds. At low LSD doses (20 micrograms), complex geometric patterns appear over physical objects with eyes open and vivid inner visuals with eyes closed. Effects intensify with dosage and can include complex hallucinations. The experience can be endlessly fascinating and focussed on small details of the visual experience. There may be a confusion of sensory inputs where sounds appear to be colours or words are perceived as tastes - a phenomenon known as synesthesia. A ‘bad trip’ is often associated with fear, panic and paranoia.
Dissociatives include ketamine and phencyclidine induce analgesia and amnesia. Dissociation of sensory input can cause derealisation, the perception of the outside world as being dream-like, vague or unreal and depersonalisation, feeling disconnected from yourself, feeling unreal, able to observe your own actions.
Deliriants include atropine, scopolamine, over the counter anti-histamines such as dimenhydrinate, and plants of the nightshade family, such as belladonna. As the name suggests these compounds cause a state of delirium, characterized by confusion, agitation, often frightening hallucinations, and amnesia. There may be detachment from reality, including odd behaviours like interacting with imaginary objects.
High quality research on treatments for psychedelics is lacking, and so practitioners need to be inventive in applying the principles of effective treatment…
Stabilisation
Psychedelic drugs do not have withdrawal syndromes which characterise most addictive drugs. The addictive potential tends to be low partly because there are only mild or zero withdrawal symptoms but also the experience is variable depending on the circumstances: feeling low, unsafe or anxious may foreshadow a bad experience. The effects of atropine and deliriants is unpleasant and so they are not used as recreational drugs. The effects of ketamine are short lived and mood enhancing making it potentially addictive.
So, initial stabilisation is unlikely to be problematic with the help of symptomatic medication.
Hallucinogen Persisting Perception Disorder and psychosis
Spontaneous ‘flashbacks’ of experiences from a psychedelic trip, occurring without having taken the drug are common. They are typically visual distortions like seeing halos or trails around objects, can occur weeks, months, or even years later. While often brief and mild, they can be distressing for some individuals.
Psychedelics can trigger a long-lasting psychotic state, especially in individuals with a pre-existing history or family history of mental health conditions like schizophrenia or bipolar disorder. Symptoms include disorganized thinking, paranoia, severe mood disturbances, and visual hallucinations that continue long after the drug's effects have worn off.
Long-term or heavy use may be associated with increased rates of anxiety, depression, and a lack of motivation. The powerful emotional experiences during a ‘bad trip’ can also lead to lasting psychological distress.
It may be that regular use of psychedelics can cause a ‘rewiring’ of the brain which underpins these mental health problems which are best managed with treatment as usual for the psychiatric disorders.
Relapse prevention
Relapse prevention medication...
There are no medications specific to psychedelics for relapse prevention - no blocking drugs for example. There are case studies - see treatment outcomes page.
Where someone is experiencing persistent mental health problems these should be managed with treatments as usual.
The craving for ketamine can be a powerful trigger for dependent use - craving for hallucinogens is unusual. If the use of psychedelics has become problematic because of physical or psychological harms or dependence then an abstinence relapse prevention plan should be considered. What might trigger further use?
in the short term
peer pressure for social/recreational use
spiritual or ritual practices
low mood (especially if psychedelics have lifted mood)
in the long term
persistent mental health problems (although unlikely to benefit)
Rating high risk situations is the first task in a relapse prevention programme. Once identified and rated for the degree of temptation and the individual’s belief in their coping ability, new coping strategies can be identified, practised and implemented in real life.
Coping skills is a core session of iSBNT…
Lifestyle change
Beyond recreational use psychedelics, taken in safe environments, have a long history of promoting transcendental, spiritual experiences, healing, and personal growth. These may be cherished behaviours that are felt to be beneficial and safe and, therefore, need sensitive reflection.
Psychedelics have a more chequered history in enhancing psychotherapies: they work by unblocking suppressed thoughts and emotions and are used in the treatment of resistant depression, PTSD and other psychiatric disorders. Nonetheless relief from psychological distress may be an important part of a lifestyle.
The goals of lifestyle change may turn out to be complicated depending on why an individual is using psychedelics. As for other drugs social treatments are most likely to be effective, for users, their family and friends, and other approaches can be effective provided that they are well structured and well delivered. Contingency management and other behavioural approaches are effective.
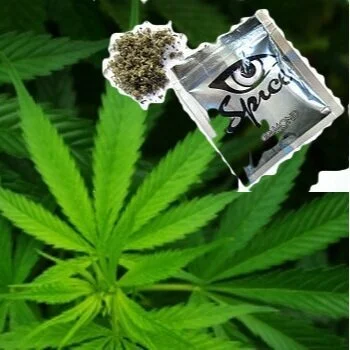
Harm reduction
Generic harm reduction measures to improve health and wellbeing are to be applied throughout treatment. There are no specific harm reduction measures for psychedelics but users must be informed of the physical and mental health harms.
Watch this slide show by Dr Duncan Raistrick to learn more about harms and harm reduction…
Duncan Raistrick is a Consultant Addiction Psychiatrist
effective interventions…